Frank Aviles, Jr, PT, CWS, FACCWS, CLT-LANA, ALM, AWCC, MAPWCA
Hyperbaric Physicians of Georgia
Natchitoches Regional Medical Center
Improving Patient Access to Care at Home
As our population continues to live longer, we face a plethora of challenges including an expanding number of people with increasing number of comorbidities, nonhealing wounds, a changing delivery of care model, and limited access to care to name a few. These challenges may be compounded by several health care disparities, including difficulty obtaining appropriate care, mobility, transportation issues, and decreased adherence, which can lead to poor outcomes.
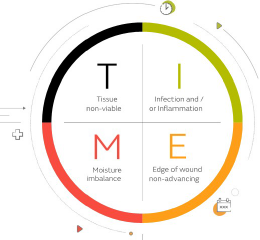
Chronic, non-healing wounds are a significant burden to the healthcare system, and often require the implementation of advanced interventions or modalities to address local and/or systemic factors interfering with the healing progression. The critical key element that is usually missing in these chronic wounds is Oxygen. While acute hypoxia is a necessary step after an injury, chronic hypoxia can stall the natural healing process.
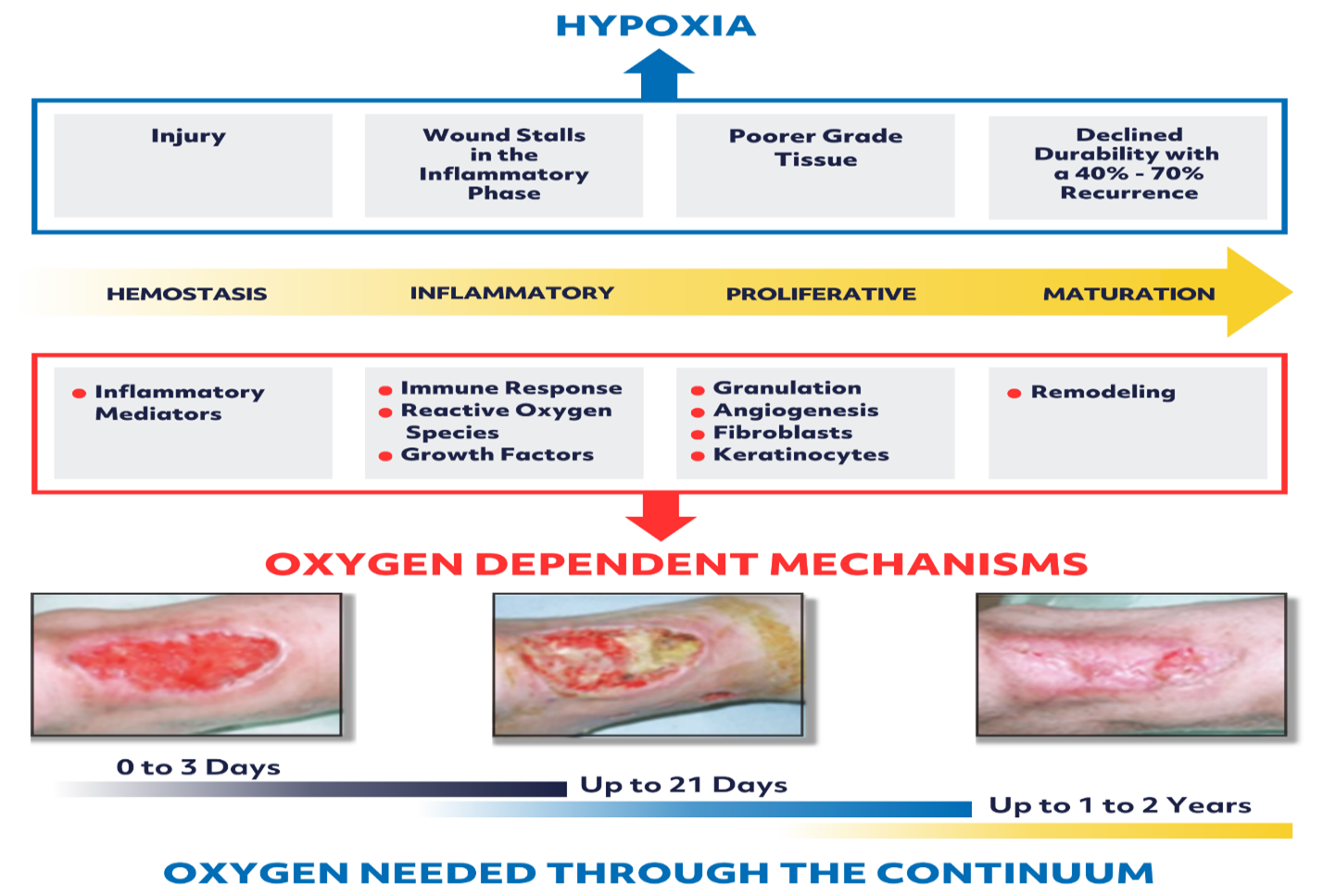
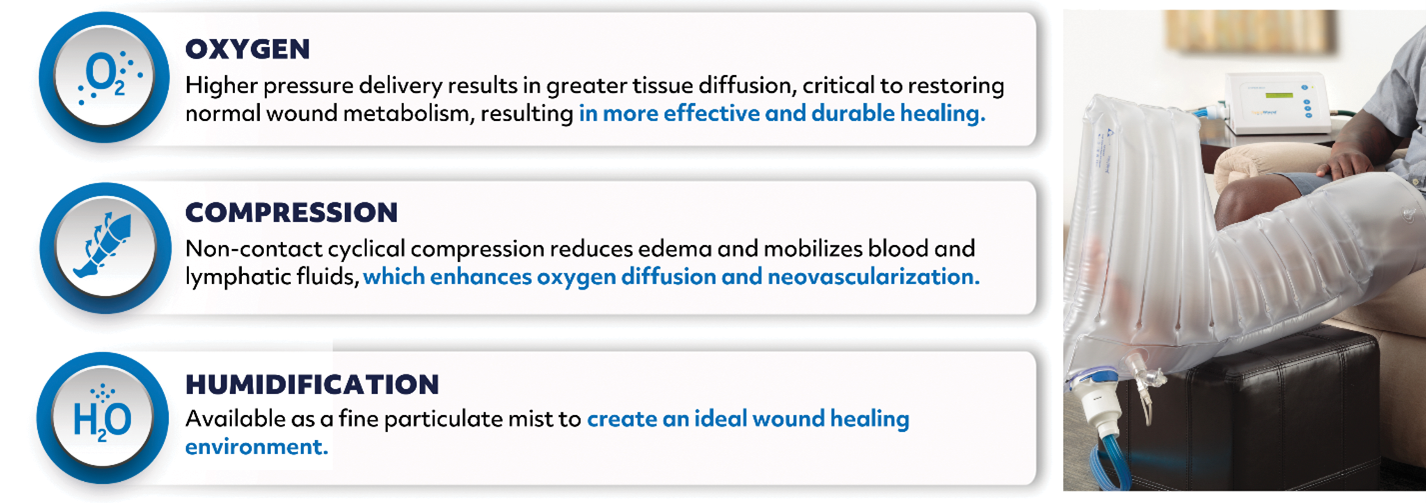
Cyclically Pressurized Topical oxygen therapy (CPTOT) is an advanced modality that has been proven to overcome the chronicity of wounds and push them towards sustained closure by combining three core components.
Studies by Fries et al.1, indicated how CPTOT can increase the level of oxygenation to the wound bed achieving an acceptable level for healing within 4 minutes. The overall body of evidence continues to grow and there are now, robust controlled studies demonstrating its utilization in progressing chronic diabetic foot ulcers (DFU’s) and venous leg ulcers (VLU’s) to more durable healing, resulting in decreased wound recurrence, avoiding amputations, and reducing hospitalizations.
The American Diabetes Association recently awarded topical oxygen therapy (TOT) an “A” rating evidence-based recommendation in their 2023 Standard of Care Guidelines2. The International Working Group on the Diabetic Foot (IWGDF) in their 2023 updated Guidelines3, stated that based on the high level of evidence, stated to “consider the use of TOT as an adjunct therapy to standard of care (SOC) for wound healing in people with related foot ulcers where SOC alone has failed”. In January 2023, Diabetes Care, Standards of Care in Diabetes2, recommends topical oxygen therapy as one of the proven modalities for treating chronic diabetic foot ulcers that have failed to heal with optimal standard of care alone.
Topical Wound Oxygen (TWO2) from AOTI, Inc., is the only marketed CPTOT device, which has an extensive body of clinical evidence to support its more durable healing of chronic non-healing and acute complex wounds thus improving the quality of life for patients and providing cost savings benefits to payers.
TWO2 can be applied anywhere on the body either via an “extremity chamber” or a “multi patch” providing a higher-pressure oxygen delivery to the treatment area, combined with non-contact cyclical compression, and humidification.
An important consideration is that TWO2 can be applied over most wound dressings, total contact casts (TCC), and compression dressings without affecting the delivery of oxygen to the wound bed. Additional benefits are as follows:
· It is utilized by the patient at home which increases access to care for those with limited provider access and for people with trouble traveling. This was noted in rural areas as well as during the Covid-19 pandemic thus improving outcomes.
· Treatment in the home, patients may have increased support and reduced care burden on family.
· Ongoing weekly outpatient clinic visits and treatments for standard wound care are not altered.
· Allowing the patient to be an active participant in their treatment based on this patient centered focused environment. Patients are more likely to follow their treatment at home when they are an active participant by understanding the seriousness of their problem and associated risks.
Studies looking at patient satisfaction in the home have shown the level of satisfaction improves as absence of difficulties with transportation, waiting time for treatment, cost savings, are alleviated with resulting improvements in their quality of life.
In summary, TWO2 is a proven multi-modality therapy that is applied by the patient at home to deliver effective levels of oxygen and non-contact cyclical pressure to help heal chronic wounds that are stalled in the inflammatory stage, resulting in reduced hospitalizations and decreased amputation rates. This is a true home-based intervention that will complement clinic treatments to improve outcomes and patient satisfaction for all hard to heal wounds.
References
1. Fries RB, Wallace WA, Roy S, et al. Dermal excisional wound healing in pigs following treatment with topically applied pure oxygen. Mutat Res. 2005 Nov 11;579(1-2):172-181.
2. Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer Billy S. Collins, Christopher H. Gibbons, John M. Giurini, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary Lou Perry, Priya Prahalad, Richard E. Pratley, Jane Jeffrie Seley, Robert C. Stanton, Jennifer K. Sun, and Robert A. Gabbay, on behalf of the American Diabetes Association. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes 2023. Diabetes Care 2023; 46 (Suppl. 1): S203-S215 | https://doi.org/10.2337/dc23-S012.
3. The International Working Group on the Diabetic Foot (IWGDF) Wound Healing Guideline, 2023, www.iwgdfguidelines.org.