|
FRONTIERS The Quarterly Newsletter of the American Academy of Home Care Medicine | Winter 2022
MODELS OF CARE AND HEALTH POLICY
Social Determinants of Health: Investing in Access and Prevention
JUNE LELAND, MD, MBA
MEDICAL DIRECTOR, HOME BASED PRIMARY CARE, JAMES A. HALEY VA, ASSOCIATE PROFESSOR, MORSANI COLLEGE OF MEDICINE AT THE UNIVERSITY OF SOUTH FLORIDA COLLEGE OF MEDICINE
Social determinants of health (SDOH) are conditions in the environments where people are born, live, learn, work, play, worship, and age. These circumstances are shaped by the distribution of money, representation, and resources at global, national, and local levels. They have wide-ranging effects on health, function, and quality-of-life outcomes and risks. They include the five categories pictured below:

Economic Stability
The national poverty rate increased between 2019 and 2020 from 10.5 percent to 11.4 percent, due in part to the COVID-19 pandemic. Poverty rates are over twice as high for Black (19.5 percent) and Hispanic Americans (17 percent) than for non-Hispanic white (8.2 percent) and Asian Americans (8.1 percent). Foreign-born non-citizens had twice the poverty rates as naturalized citizens, and the poverty rates for the disabled (25 percent) were roughly the same as for those without a high school diploma (24.7 percent).
For the aging population, Economic Stability encompasses having adequate finances to meet their needs as well as access to financial planning. According to a 2018 survey, 39.3 percent of those over 65 were satisfied with their finances, but 16.9 percent reported difficulty paying bills, 32.6 percent were concerned about getting trustworthy financial advice, and 25 percent were concerned about being taken advantage of financially. Among adults 65 and older, 10 percent reported food insecurity, but that more than doubled to 22.9 percent for low-income households. Food insecurity can lead to tradeoffs between basic needs, and more than 22 percent of older adults were moderately or very concerned about affording nutritious food or having to make tradeoffs between food and other necessities as they age. While concern varied slightly by age group, the most concerned were those who were already struggling. Almost 40 percent of older adults expressed concern about being able to afford to stay in their home or make repairs to their homes as they age, including 55.5 percent of low-income older adults compared to 30.1 percent of those with higher incomes. A higher percentage of older adults living alone at the time of the survey expressed concern, 48.6 percent as compared to 36.2 percent of those living with others. In 2019, 5.2 million seniors (7.1 percent of all seniors) faced hunger.
- 63 percent of seniors visiting food banks say they have to choose between food and medical care.
- Hunger takes a severe toll on seniors' health and nutrition, putting them at risk for chronic health conditions like depression, asthma, and diabetes.
- Millions of seniors qualify for monthly grocery assistance through SNAP, but only 42 percent receive SNAP benefits.
- Some seniors are more likely to face hunger, including seniors who identify as Black or Latinx, seniors who live in rural areas, seniors with disabilities, and seniors who are renters.
Related reading: The State of FoodRx Programs
Education Access and Quality
People with higher levels of education are more likely to be healthier and to live longer. Barriers to accessing quality education include lack of high performing schools and the cost of a college education. Disabled and low-income children and those who experience social discrimination may struggle with math and reading and are less likely to graduate from high school or to attend college. This in turn leads to lower income which is linked to poor health. The goal for Healthy People 2030 is to increase educational opportunities and help children and adolescents do well in school. The approach includes improvements in education for preschoolers, children, and adolescents as well as disabled students. It also focuses on the quality of training for educators. For an aging population, there is evidence that education is important for people in terms of improvement of longevity and reduction in incidence of disability. Lifelong learning appears to have a conserving effect on wellbeing, health, and vulnerability in the aging population.
Healthcare Access and Quality
Limitations to quality health care services include lack of insurance, lack of primary care access, and lack of availability of medical care in a given area. The Healthy People 2030 goal is to increase access to comprehensive, high-quality health care services. Home health care and the expansion of telemedicine services have increased access to primary and specialty care under Medicare and private insurance, but there are still barriers to care. Internet access can be an issue, as well as lack of information about how to access resources. This is linked to social and community contacts. Access to Medicaid services remains limited by funding and by geographic area. The NIH proposed strategic directions for research 2020-25 which includes understanding health disparities related to aging and to develop strategies to improve the health status of older adults in diverse populations. NIH goals include:
- Identify and understand environmental, social, cultural, behavioral, and biological factors that create and sustain health disparities among older adults.
- Develop strategies to promote active life expectancy and improve the health status of older adults in diverse populations.
- Develop and implement strategies to increase inclusion of underrepresented populations in aging research.
- Support research on women’s health, including studies of how sex and gender influence aging processes and outcomes.
Preventative care, consistent primary care, the ability to obtain prescriptions, health literacy, language barriers, EMR challenges across care settings, and lack of insurance coverage for vision, hearing, and oral health remain problematic for elders. As more Americans become eligible for federal entitlement programs like Medicare and Social Security, spending reductions and tax increases may follow, with the potential of further limiting services.
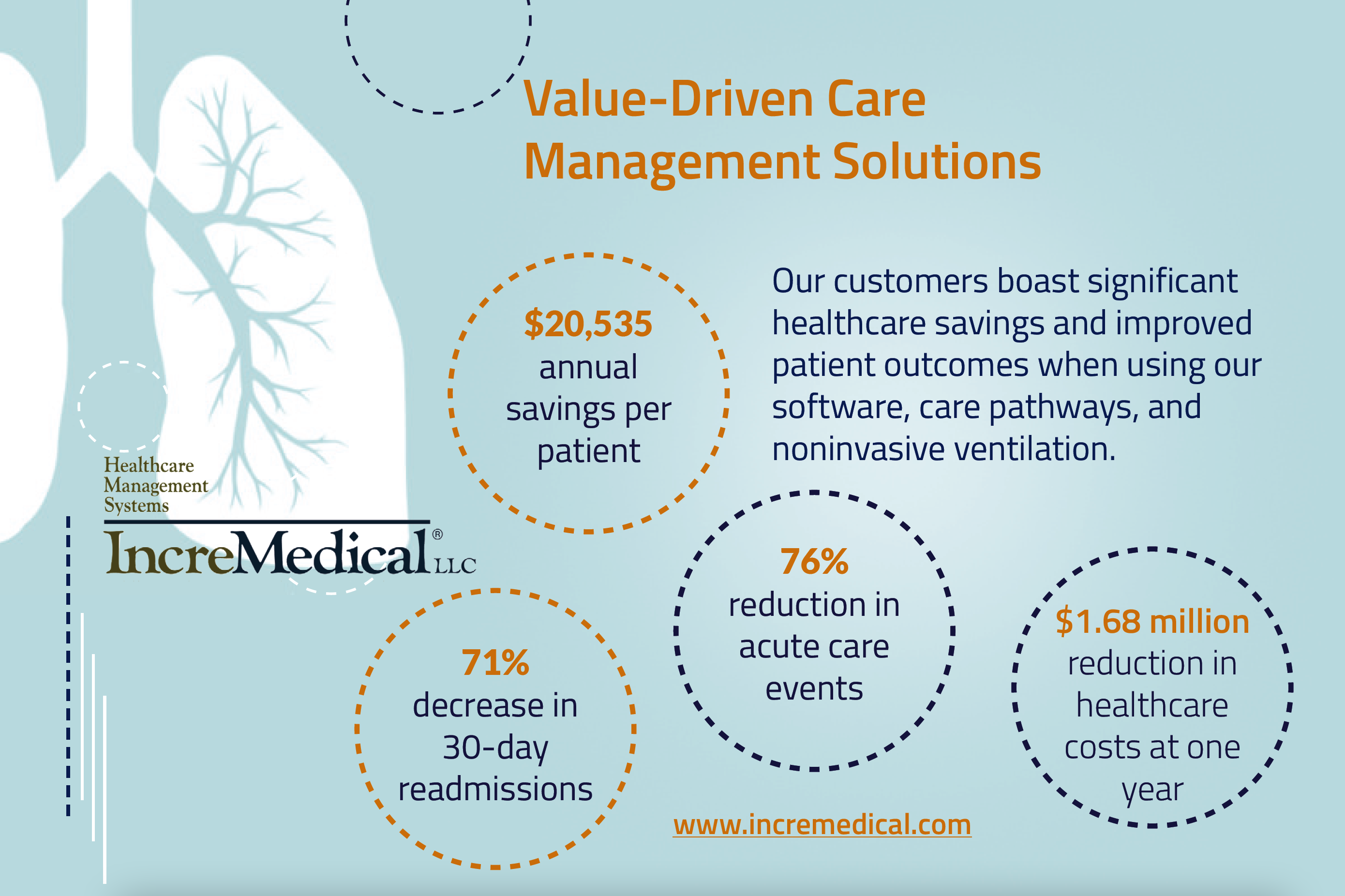
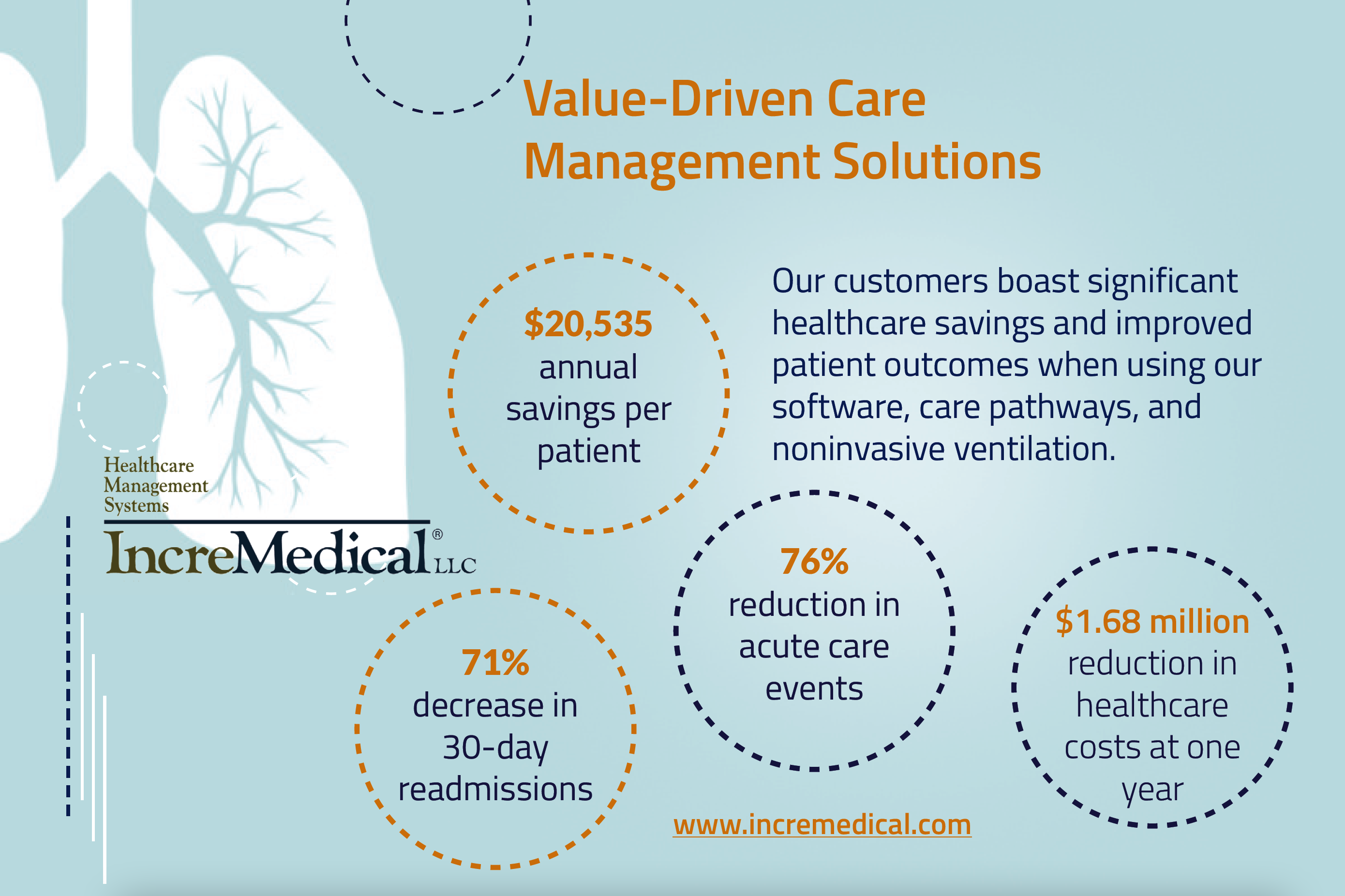
Advertisement
Neighborhood and Built Environment
Neighborhoods that are unsafe because of violence, air or water pollution, lack of outdoor space, or inadequate infrastructure such as transportation and broadband access present barriers to health. The Healthy People 2030 goal is to create neighborhoods and environments that promote health and safety. Another goal is to decrease the proportion of families spending more than 30 percent of their income on housing and to make housing more accessible to people with disabilities. Related goals include reducing emergency visits for asthma and COPD, along with minimizing hearing loss from noise exposure. The $1.2 trillion infrastructure bill that passed in November 2021 delivers $550 billion of new federal investments in America's infrastructure over five years, including money for roads, bridges, mass transit, rail, airports, ports, and waterways. The package includes a $65 billion investment in improving the nation's broadband infrastructure and invests tens of billions of dollars in improving the electric grid and water systems. Another $7.5 billion would go to building a nationwide network of plug-in electric vehicle chargers, according to the bill text.
Environment has a strong correlation to individuals’ access to exercise and physical recreation. Exercise options are limited for many elders because of expense or unavailability of group settings and lack of resources for cable television as well as subscription services needed to access health and exercise related programs such as “Sit and Be Fit” or health education topics. Access to internet-based programs is also subject to fees as well as equipment. Programs such a “Silver Sneakers” are offered in person with some insurance plans and are also available online. Health care providers may lack experience in providing an exercise prescription or lack familiarity of programs available in their communities. Older adults enjoy bicycling and walking for outdoor activities in livable communities as a key to staying healthy and active. Cycling increased as an outdoor activity during the pandemic. However, traffic deaths for older cyclists and pedestrians are a disproportionate and growing share of all motor vehicle-related fatalities. In fact, people aged 55 to 64 have the highest per capita rates of being killed while biking and walking. Florida, a state with one of the highest proportions of senior residents, continues to have the highest per capita fatality rate for cyclists.
Social and community context
People’s relationships and interactions with family, friends, co-workers, and community members can have a major impact on their health and well-being. The goal of Healthy People 2030 focuses on helping people get the social support they need in the places where they live, work, learn, and play.
Many people face challenges and dangers they can’t control — like unsafe neighborhoods, discrimination, or trouble affording the things they need. This can have a negative impact on health and safety throughout life. Areas for improvement include increased health literacy and health communication, including electronic access. Loneliness and isolation can worsen the risk of death and chronic conditions for older adults. More than one in five older adults were frequently or often lonely at the time they were surveyed. Among older adults experiencing loneliness, nearly half (47 percent) were moderately or very concerned about living alone as they age. About 30 percent of older adults were concerned about living independently as they age; those who were living alone at the time of the survey expressed the greatest concern (41 percent). Reliable transportation is a key factor governing independence and aging in place. Older adults with reliable access to transportation are better able to get to medical appointments, run errands, and attend social events. Lack of transportation can present a significant barrier in some communities. Lack of trauma-informed care can also lead to trauma in special populations. For example, more than 39 million people in the U.S. are age 65 years or older, including 2.4 million people who identify as lesbian, gay, bisexual, or transgender (LGBT). As the baby boomer generation ages, the older adult population will increase from 12.8 percent to an estimated 19 percent in 2030. LGBT older adults may disproportionately be affected by poverty and physical and mental health conditions due to a lifetime of unique stressors associated with being a minority and may be more vulnerable to neglect and mistreatment in aging care facilities. They may face dual discrimination due to their age and their sexual orientation or gender identity.
There’s Work to be Done
In order to achieve the goals of Healthy People 2030, health care providers should be encouraged to recognize and implement screening for SDOH during visits. This can include screening for food insecurity, social supports, housing, transportation, and social isolation, especially among those with low incomes. Referrals to community services can be made where appropriate. Policymakers should be encouraged to address SDOH at every level of community and to fund and expand programs for the aging population and include streamlining and simplifying enrollment for available programs. Funding for programs that address SDOH should be encouraged. Reduced cost senior housing and reduced prescription costs would make more money available to seniors for food and other needs. Transportation services would allow elders to increase access to a range of services, including social supports to reduce loneliness and promote lifelong learning. Support for elders and their caregivers with expanded affordable home health services not requiring a skilled level of care would improve care for the homebound and families who support them.
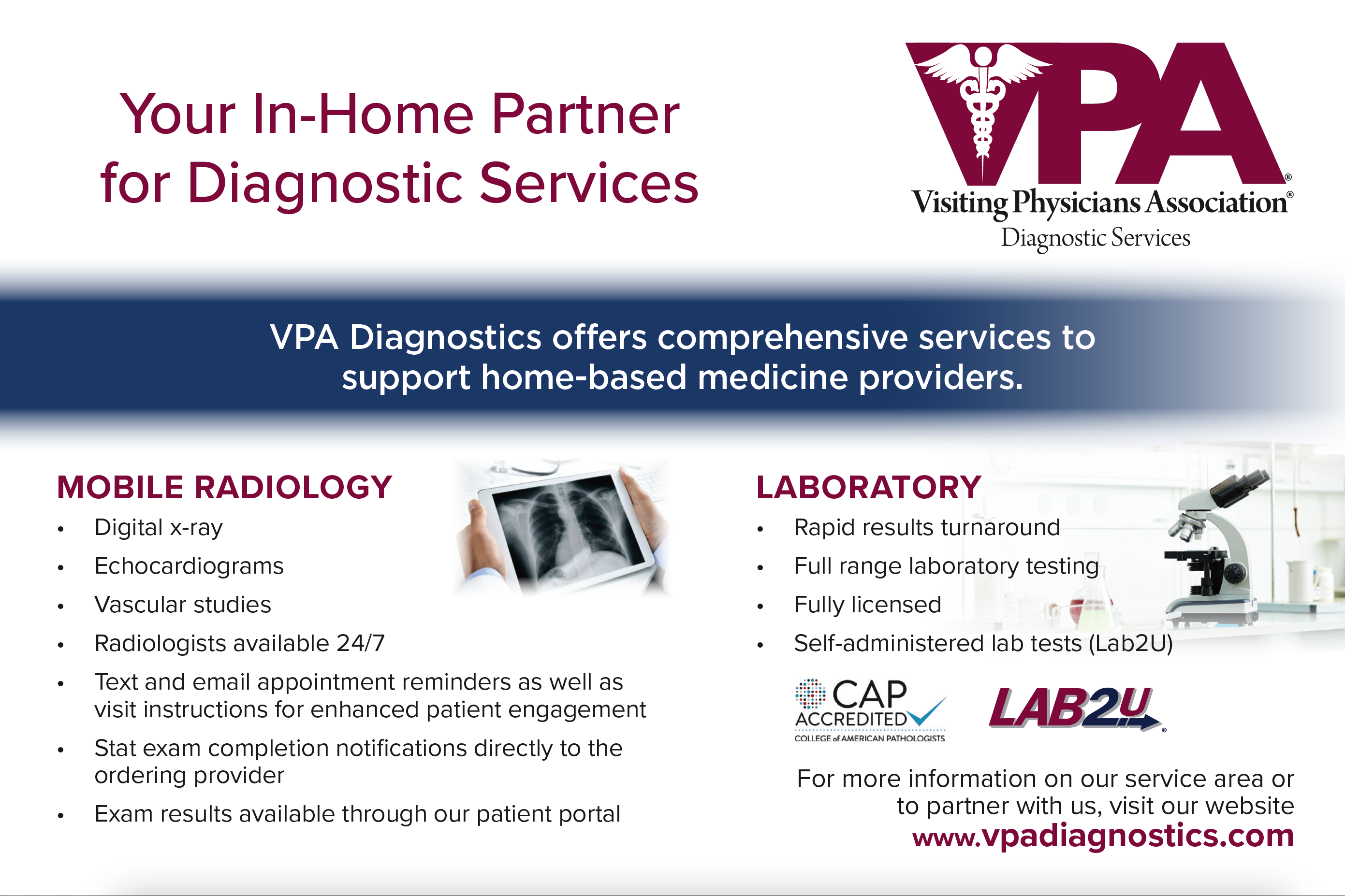
Advertisement
Back to Frontiers >
|