- House Call Finder
- ACO
- Join & Get Involved
- Public Policy
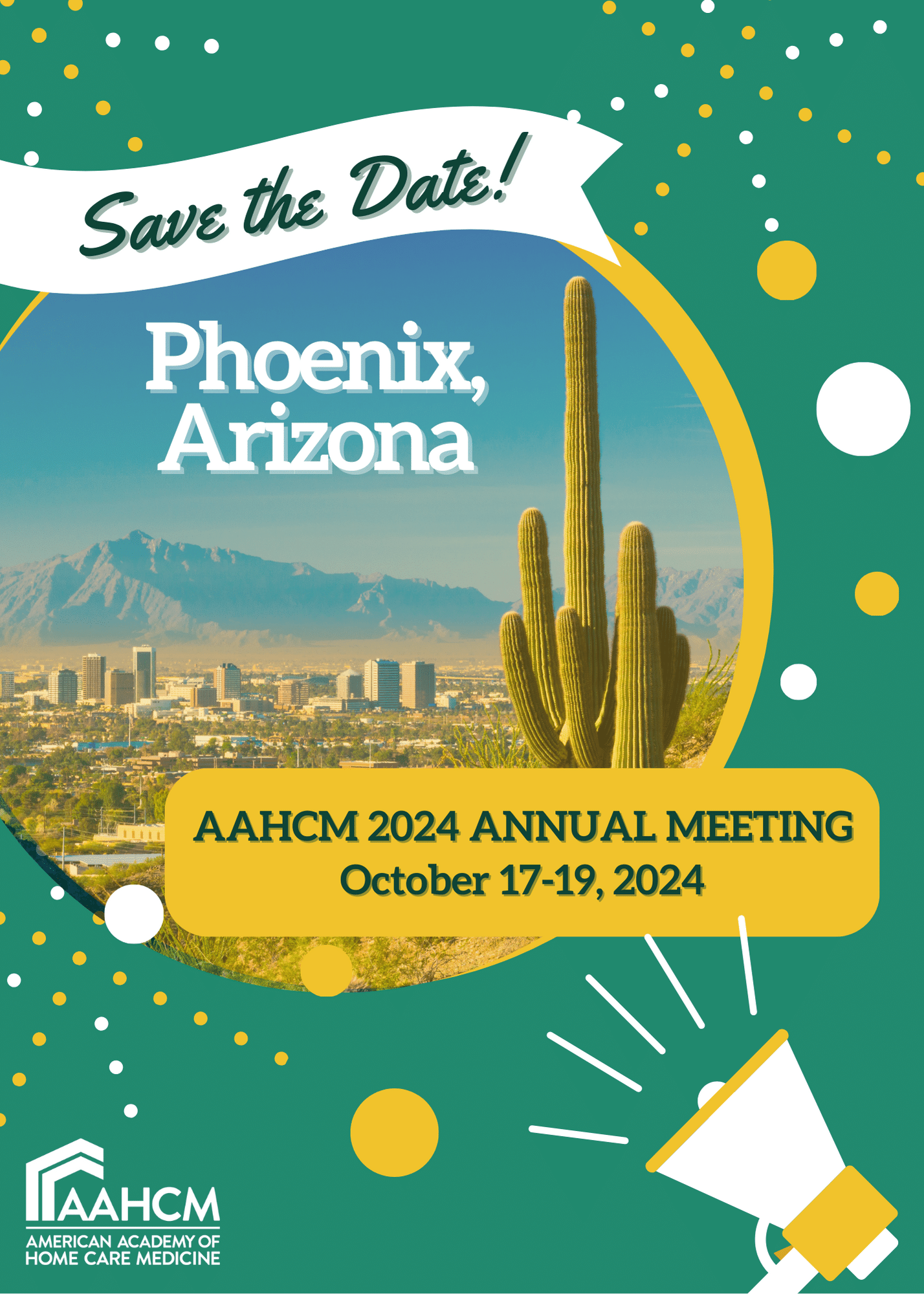
- Events
- Education
- Partners
- About
Welcome to the American Academy of Home Care Medicine
|
THE POWER OF HOME CARE MEDICINE |
CONNECT WITH OTHER MEMBERS |
|
Learn about what makes home care medicine so vital through videos, a white paper, FAQs, & more! Resources |
Engage with other AAHCM members in the Community Forums. Get Involved |
Updates
Click HERE to see our latest Public Policy E-Briefing.